Improving Quality of Education Inside and Outside the Classroom
At ACPHS, the PharmD IPE student experience progresses from foundational knowledge in the first year to practical application in the fourth and final year by following a stepwise approach. IPE student experiences are integrated across all four years of the Doctor of Pharmacy including both didactic (classroom) and experiential (real world) aspects.
To offer IPE experiences, external partnerships with other health professions schools are required. Students at ACPHS will work with other health professions students from our partner institutions, including Albany Medical College, Russell Sage College, SUNY Erie Dental School, and Excelsior University Nursing.
In April 2025, the Accreditation Council for Pharmacy Education (ACPE) reviewed our IPE Program and granted it a Commendation, which is a special recognition for excellence for our “highly collaborative and successful IPE program.”
Learn More:
Interprofessional Education Vision, Mission, Goals
ACPHS will graduate pharmacists who actively collaborate with other health professionals to provide and promote patient centered care.
The mission of IPE at ACPHS is to provide every student multiple opportunities to learn about, from and with other health professions. Through these experiences, students will develop competencies (goals) in each of the four recognized IPE domains. Through local and regional affiliations, our students and faculty will provide leadership to build stronger healthcare teams and thus improve the care of their patients.
Facilitate development of student competency in each of the four Interprofessional Education Collaborative IPE competencies prior to graduation.
- Values and Ethics: Work with team members to maintain a climate of shared values, ethical conduct, and mutual respect.
- Roles and Responsibilities: Use the knowledge of one’s own role and team members’ expertise to address individual and population health outcomes.
- Communication: Communicate in a responsive, responsible, respectful, and compassionate manner with team members.
- Teams and Teamwork: Apply values and principles of the science of teamwork to adapt one’s own role in a variety of team settings.
Support faculty engagement with IPE through teaching, scholarship, service, and faculty development.
Communicate the IPE program to internal and external stakeholders.
Serve as a community partner and collaborator with other local health professions schools to offer high quality IPE student experiences.
“When asked what drew her to ACPHS, School of Pharmacy Dean, Elena Umland, PharmD stated, “...a personal passion, is the further growth and development of the interprofessional education (IPE) elements of the curriculum through collaboration with Albany Medical College, our own programs of cytotechnology, psychology, public health, nursing, physician assistant and the programs of our partner Russell Sage College, occupational therapy, physical therapy and others.”
 Elena Umland, School of Pharmacy Dean
Elena Umland, School of Pharmacy Dean
Interprofessional Education @ACPHS
Discover the wonderful benefits of the interprofessional education program and understand why it’s such an important part of learning.
Student Experience Timeline
Tier Key:
- Tier 1 Foundational: What is IPE? How does it work in health care systems? Why is it important?
- Tier 2 Simulated Patient Care: Teamwork in a classroom using simulated patient cases (e.g. Team-based, case-based discussions)
- Tier 3 Indirect Patient Care: Clinically reason together about real patient care in a classroom setting; independent review of data in preparation for class
- Tier 4 Direct Patient Care: Co-interview and examine patients together; clinically reason together; co-create, implement, and follow up on patient care plans
| PharmD Year | Tier | IPE Experience | Course | healthcare professionAL Collaborator |
|---|---|---|---|---|
| P1 | 1 | IPE Health Professions Panel |
Foundations of Pharmacy | Physician Assistant |
| P2 | 3 | Dental Patient Medication Evaluation | Patient Care Workshop 1 | Dental Hygienist |
| 2 | Medication Reconciliation | Patient Care Workshop 2 | Medical | |
| P3 | 2 | Geriatric Teaching Day | Patient Care Workshop 3 | Medical |
| 2 | Opioid and Addiction Teaching Day | Patient Care Workshop 4 | Medical | |
| 1 | Scleroderma | PTP Rheumatology/Oncology | PT, OT, RN, Nutr., Psych, PharmD, Public Health | |
| 1 | Amyotrophic Lateral Sclerosis (ALS) | PTP Neuro/Psych | PT, OT, RN, Nutr., Psych, PharmD, Public Health | |
| P4 | 3 | Pharmacy Interprofessional Experience (PIPE) | APPE Rotations | Medical |
| 4 | Patient Care Teams | APPE Rotations | Various per rotation site |
The inclusion of IPE in national and ACPHS domains highlights its critical role in the pharmacy student experience.
National ACPE accreditation requirements include team dynamics, team education and team practice. It also involves core Entrustable Professional Activities (EPAs) for new pharmacy graduates, particularly in the interprofessional team member domain. The Center for the Advancement of Pharmacy Education domains cover several areas, such as learner development, problem-solving, collaboration, advocacy, communication, self-awareness, leadership, innovation and professionalism. Moreover, the Pharmacists’ Patient Care Process (PPCP) involves five essential steps: collect, assess, plan, implement, and follow up, which includes monitoring the patient’s progress.
Albany College of Pharmacy and Health Sciences has laid out a strategic plan that focuses on five key areas:
- Academic Excellence
- Quality Student Experience
- People and Culture
- Engaging with Communities
- Financial Strength & Stewardship
The College also has a set of core values that guide its activities and interactions. These values include student-centered, integrity, respect, collaboration, community, and excellence. Student-centeredness involves mutual respect and positive and engaging interactions. Integrity is about honesty, trust, principles, accountability, and responsibility, and it requires all members to behave in a way that reflects positively on themselves and the institution. Respect demonstrates professional courtesy and exhibits care, concern, and consideration for others. Collaboration breaks down silos and encourages teamwork, while community involves a shared sense of purpose and identity. Excellence is consistently striving to do the very best work for our students and for all within our campus community. Appreciating our students and colleagues for their work ethic and commitment to excellence.
As per the ACPE accreditation standards, all pharmacy schools must create an IPE student experience.
- Interprofessional team dynamics – All students are expected to show their competence in interprofessional team dynamics. This includes the ability to articulate the values and ethics that underpin interprofessional practice, engage in effective interprofessional communication (e.g., conflict resolution and documentation skills), and honor their interprofessional roles and responsibilities. The didactic and Introductory Pharmacy Practice Experience (IPPE) components of the curriculum introduce, reinforce and provide opportunities for practice of interprofessional team dynamics. Competency in interprofessional team dynamics is then demonstrated in Advanced Pharmacy Practice Experience (APPE) practice settings.
- Interprofessional team education – The curriculum enables collaboration and quality patient care by providing students with interprofessional educational activities. These activities help students learn from and work with other healthcare team members and understand their abilities and competencies, as well as their scope of practice. Note that some activities may involve simulations, but not all.
- Interprofessional team practice – As competent healthcare team members, all students participate in providing direct patient care and engaging in shared therapeutic decision-making. They engage in experiential educational activities with prescribers/student prescribers and other healthcare team members. These activities include face-to-face interactions and are designed to improve interprofessional team effectiveness.
Advanced Pharmacy Practice Experiences (APPEs)
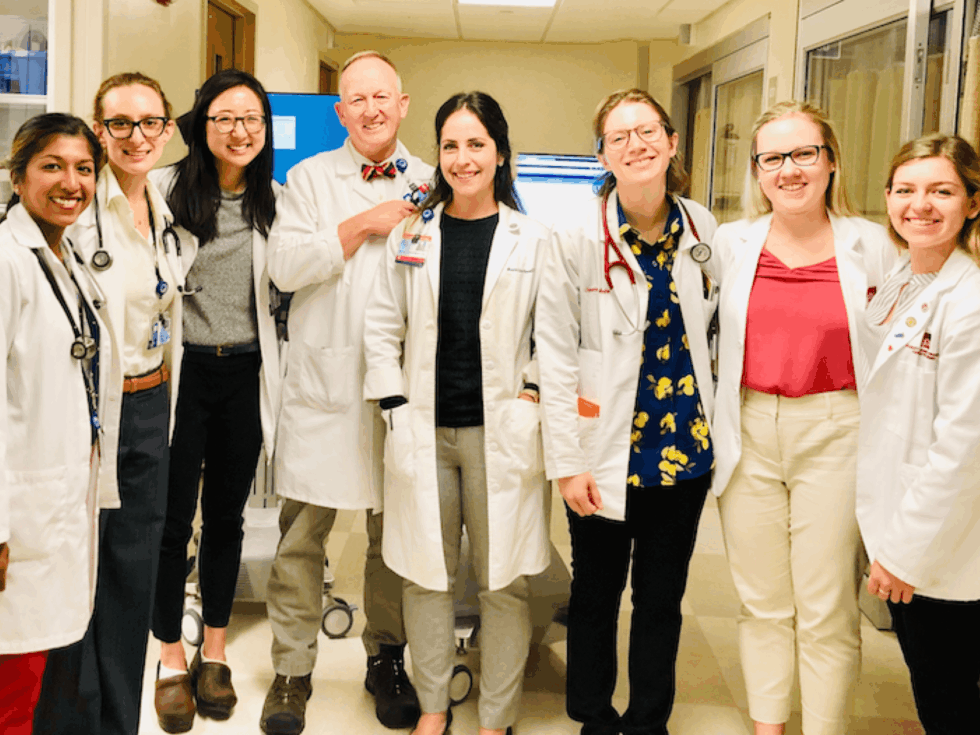
During their APPEs, all students participate in interprofessional education. These experiences provide students with the opportunity to practice their interprofessional collaboration skills by working together with students from other health professions in real-world settings to solve patient care problems. An example of such an experience is the Pharmacy Interprofessional Experience (PIPE) at Albany Medical College. Here, pharmacy and medical students collaborate in small groups to evaluate real patients admitted to Albany Medical Center Hospital. They then develop recommendations to improve the patient's care, which can be implemented.
For more information on Pharmacy Interprofessional Experience (PIPE) please review the following materials:
Meet Our PIPE Program Co-Director
Joseph T. Wayne is the PIPE Program Co-Director along with Amanda Engle, BS, PharmD, BCPS and David Butler, PharmD, BCPS, BCIDP Assistant Professor, Department of Pharmacy Practice.
 Joseph T. Wayne, MD MPH MACP FRCP
Joseph T. Wayne, MD MPH MACP FRCP
Professor of Internal Medicine & Pediatrics
Clerkship Director for Internal Medicine
Associate Program Director, Internal Medicine
Department of Internal Medicine
Day in the Life
Pharmacy Students Caring for Patients on an Interprofessional Team
“Interprofessional education is a crucial part of the curriculum at ACPHS. During my inpatient internal medicine rotation at Albany Medical Center, I had the opportunity to be part of an interprofessional disciplinary team. Being part of this team made me realize the importance of my role as a student pharmacist in patient care. By effectively contributing to improving patient care and paying attention to every detail, we enhanced trust and respect among team members. Seeing the impact of our contributions on patient care was truly fulfilling.”
—Kayla Wesley, Doctor of Pharmacy Class of 2024
Hello! My name is Kayla Wesley, Doctor of Pharmacy Class of 2024.
Interprofessional education is a component of the curriculum here at ACPHS. I also had the pleasure of participating on an interprofessional disciplinary team during my inpatient internal medicine rotation at Albany Medical Center.
As student pharmacists, we played an important role in elevating patient care via collaborative relationships with the medicine team. Our teams were varied with experience, consisting of the attending physician, medical residents, medical interns, and 3rd year medical students. The pharmacy half consisted of our clinical pharmacist preceptor Dr. Engle, PGY-2 pain and palliative care pharmacy resident Dr. Dean, and us P4 student pharmacists. Over the course of our 6 week rotation, the medicine team members rotated every couple of weeks, so we got to experience many different teaching styles and learned how to adapt our communication skills to fit each team.
Each week, us pharmacy students paired up with a new 3rd year medical student. Every day was different with new patients and follow-ups, but the days followed a similar workflow. During a typical day, us pharmacy students would arrive on the floor by 7AM each morning and chat with our respective medical students to see what new patients they had picked up. Some patients could have been admitted to the internal medicine floor from the emergency room, others could have been stepped down from the ICU, or some could have come from another hospital; each patient had a different story. As part of the pharmacy team, we would “work up” our assigned patients which meant consolidating their story to explain why they were here, what acute problems they had, and what medical interventions and medication changes we could do to help resolve those problems. This challenged us to apply the knowledge we had gained from our didactic coursework at ACPHS, and it was exciting to see how everything we have learned could be utilized in practice for real patients.
While working up our new patients, we also made time for reviewing our other patients from the days prior. By around 8:15, our preceptor Dr. Engle would arrive on the floor, and we would take turns presenting our newly admitted patients to her. We would run through the patient’s list of problems and our recommendations for them, whether it was a medication change, initiating or discontinuing a medication, obtaining new lab values to clarify the problem, and more. After solidifying our recommendations with our preceptor, we would find our medical students again and run through our patients together, listening to each other’s perspectives and thoughts, and make a plan for what we would present to the attending physician during rounds.
Most mornings we would also attempt to complete medication reconciliations as part of our patient work-up, which entailed obtaining a list of all the medications the patient takes at home and verifying via different resources it to ensure its accuracy. We would then update the home medication list in their chart so everyone on the care team could see, and then we would compare it with what the patient was receiving during their hospitalization. Medication reconciliations were another great intervention opportunity for student pharmacists to provide recommendations—we could ensure the patient receives the medications they usually take at home or recommend making adjustments to better optimize their regimens.
Rounds started at 9AM and everyone on the team would gather for patient presentations. The medical students would go first presenting their newly admitted patient, and us pharmacy students would chime in to go over the home medications and present our recommendations to develop an effective plan with the team. After presenting the newly admitted patients, everyone would present their follow-up patients from the days prior, and then review the patients being prepared for discharge. The total number of patients under our care varied each day, but was usually between 12-17, and rounds would last 2.5-3 hours. There were countless opportunities for teaching moments during rounds between the pharmacy members and the medicine members, and it was wonderful to see how powerful it really was to be able to share knowledge and gain insight from different clinical roles.
After rounds, our pharmacy team would touch base about what we needed to accomplish in the afternoon for follow-up, then we would head to lunch. Our afternoons had the greatest variability. After lunch, we would return to the floor and start working on any tasks and questions that were not answered during rounds. Follow-up could have consisted of doing pain assessments, doing detective work on medications, checking if certain labs had resulted yet, completing medication reconciliations, and more. We would pop back in to chat with the team about any further recommendations based on our afternoon follow-up and further solidify our plans.
Participating on an interprofessional disciplinary team helped me realize the value in my clinical role as a student pharmacist. By effectively contributing our services to improving patient care and letting no detail go unmissed, we could tangibly feel the trust and respect grow between our team members. It was genuinely a rewarding experience to see the value of our contributions on patient care.
Student Testimonials
“It is a great learning experience to be able to work with medical students. Honestly, this type of interprofessional training will change the next generation of healthcare professionals. We will be more collaborative patient care providers and that is what the healthcare system needs.”
“Working alongside medical student colleagues has left me with the most meaningful impression overall. I am now a firm believer that to effectively work together as healthcare professionals, we must learn together as effective students. This will definitely affect the way in which I practice pharmacy now having completed this interprofessional experience.”
“Collaborating with a new med student each week challenged our adaptability to work with each other as interprofessional colleagues to figure out how our professions “fit” in with each other while caring for the same patients. Each week we had to find the best workflow with each other, and since everyone has a different style and approach, it was a bit jarring at times to figure out how we could each benefit each other and grow from one another.”
“Through this process, I gained a more solidified sense of other’s roles and how we could use each other as a resource. We learned to adapt to each other’s professions and execute quality patient care within a multidisciplinary team. We improved our communication with each other, settled into a smooth workflow, and executed better patient care, and then started from scratch again with new partners the following week.”
“Not all rotations have a strong interprofessional component or exposure to other health care professionals or students, but this rotation has definitely provided a wonderful interprofessional experience. It is crucial to have IPE experience to better understand the other professionals you work alongside with and find how we each fit into each other like puzzle pieces as the health care team taking care of our patients.”
“The interprofessional aspect of this experience had the biggest impact on me. Learning to work together with medical students provided me with insight into the aspects of patient care that medical students provide versus what pharmacy students provide. Understanding how our roles differed allowed me to maximize my contributions on the team and give recommendations that showcased the value of a pharmacy student. Working with the medical students also challenged me to create interprofessional relationships centered on trust and mutual respect.”
“During my experience in my inpatient internal medicine rotation, I was given the opportunity to work on an interdisciplinary team of medical students, resident physicians, student physician assistants and hospital attending physicians in an effort to build the best possible patient care plans for our patients. My focus on the medications allowed the medical students to focus on the examinations and physical aspects of the patient care, allowing me to use their assessments to guide our recommendations based on the guidelines. This experience was unlike any other experience I have had during my career as a pharmacy intern.”
Preparing you for the Practice
A standardized set of core competencies for collaborative practice exists to guide the development of programs for all healthcare professions schools in the United States.
Values and ethics – Emphasize common goal of providing high quality, patient-centered health care while demonstrating mutual respect, trust, integrity, and high standards of ethics
Roles and responsibilities – Realize students may lack an understanding of the roles and responsibilities of other health professionals
Interprofessional communication – Acknowledge hierarchy by intentionally using language to establish an equal learning environment. Create a safe and brave space wherein students feel comfortable speaking to each other and facilitators primarily listen
Teams and teamwork – Promote the benefits of interprofessional learning for teamwork and link effective team collaboration to patient care
Interprofessional Collaborative Practice
Interprofessional collaborative practice is key to the safe, high-quality, accessible, patient-centered care desired by all.
Interprofessional Education Collaborative. (2016). Core competencies for interprofessional collaborative practice: 2016 update. Washington, DC: Interprofessional Education Collaborative.
Questions?












Social